Arthritis of the Hand and Wrist
What are the predominant arthritis conditions you see in the wrist and hand?
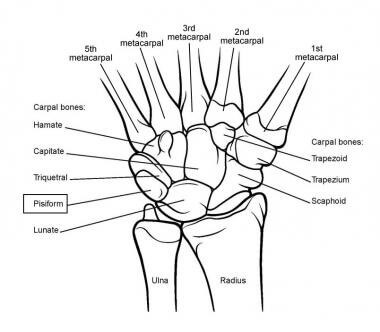
Perhaps the most common one I have seen is arthritis of the base of the thumb, also known as carpal-metacarpal arthritis or CMC arthritis (Basal arthritis). This affects the bone in the base of the thumb (metacarpal) and leads to pain of the thumb when using it for gripping such as in holding a pen or a jug of water. The arthritis affects the area between the base of the thumb and the small bone called the trapezium or between the base of the trapezium and another bone in the wrist called the scaphoid, resulting in scapho-trapezial-trapezoid arthritis (STT arthritis). Often the arthritis occurs all around the trapezium, called pan trapezial arthritis. This condition usually occurs in the middle age and is more common in ladies than in men.
What are the treatment options for arthritis in the wrists or hands?
Treatment starts with simple measures such as analgesics (Panadol, Panadeine or stronger pain killers), anti-inflammatories (Nurofen, Voltaren or other forms of anti-inflammatory medication) and then progresses to steroid injections done under ultrasound guidance, which can give short term benefit. If all that fails then the operation of choice is a trapezial excision and an interposition (placement of tendon) into the space where the bone was, so as to hold the other bones out to length. After the surgery the patient is placed in a plaster, often with a pin to hold the bone in place. The plaster and the pin are removed at six weeks, and motion is commenced.
How successful is the operation?
The operation can be very successful, and we would expect a 95-98% success rate. It does involve a plaster for a period of time and that results in an inability to drive a car while it is on, but apart from that, they are encouraged to use the hand for most activities. Most patients see significant improvement in their symptoms within three months after the surgery.
What are the risks of hand surgery?
The risks include infection, which would require antibiotics and a possible return to theatre, the risks of anaesthetics and the risk that the surgery may fail to give any benefit. There is also a scar and sometimes numbness along the side of the thumb associated with the scar, as there is a chance of a small nerve being damaged.
What other areas are affected by arthritis in the hand or wrist?

Arthritis can affect the various joints of the knuckles, such the main knuckle known as the metacarpal-phalangeal joints or the inter phalangeal joints (the knuckles further down the fingers). This is often associated with extra bone growth known as nodes and deformities of the fingers, along with stiffness. In most cases the pain is not severe with such arthritis, and when there is pain it often settles with a corticosteroid injection. The main hindrance is the deformity and the appearance of extra bone. If the joint does remain painful and has failed to respond to pain killers and anti-inflammatories or steroid injections, there are operations available.
The best operation in most scenarios is a fusion of the joint which leads to permanent stiffness of only that particular joint making it more stable. Although there are joint replacements available, these can fail (loosen) in the long term. A fusion is a stronger, more stable alternative.
Arthritis can occur in the wrist itself. The most common reason it occurs in the wrist is when there has been a fracture of the scaphoid or disruption of the ligament between the scaphoid and the bone called the lunate. This leads to arthritis at the base of the scaphoid and causes pain down along the side of the thumb but further up the wrist towards the forearm.

Treatment for this can involve analgesics, anti-inflammatories, splinting and steroid injection. If this fails, then a very successful operation is a four corner fusion. This is where the scaphoid is removed and the other four bones are fused. Whilst this does result in slightly reduced range of motion compared to a normal wrist, in those patients who require it, they often have better movement because the wrist was previously stiff due to pain. Such a procedure requires a splint for six to eight weeks after surgery and regular x-rays to make sure the bones fully unite. This can be very successful, with a success rate in the order of 90% of patients seeing improvement in symptoms and having less pain.
For more information or to book a consultation, contact us.
