
Shoulder Dislocations
Unstable shoulders are common events brought to the limelight by sporting injuries, particularly Australian Rules Football.
What is the actual pathology of the condition and how is it treated?
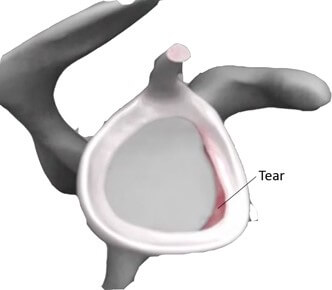
Instability of the shoulder is where the shoulder (humeral head or ball of shoulder) dislocates out of the joint (glenoid cavity or socket). The shoulder is made up of the glenoid, which is a socket in which the ball of the shoulder sits. Because of the range of motion required for the shoulder, the shoulder ball is approximately four times larger than the socket. This is best seen when looking from the anterior portal during arthroscopy, when one can appreciate how big the head is compared to the socket. When viewed this way it is no surprise that the shoulder can become unstable. To make the shoulder more stable, the body develops a tissue around the socket called the labrum. This extends a lip onto the socket to increase the size. The combination of the socket itself (glenoid) and the labrum produces a total socket which is much closer to the size of the humeral head and, along with the capsule which joins to the labrum, provides for increased stability.
In some traumatic events the ball can be pushed out of the socket tearing both the capsule and the labrum, with the labrum pulling away from the socket producing a lesion called a Bankart Lesion. As the head pops over the edge of the socket, it can be dented and this is called a Hill Sach’s lesion.
The most common episode of instability occurs when there is anterior instability, which is when the arm is thrown into the abducted externally rotated position (policeman stop position). This is the same position which occurs when a footballer goes for an overhead mark or the arm is thrown outwards when falling at speed.
Other episodes of instability occur when a shoulder is forced backwards, which can occur when falling with the arm across the chest and is also a very common event following an epileptic seizure. This leads to a posterior dislocation which can sometimes be difficult to diagnose on x-ray. Another type of instability is inferior instability which occurs when the shoulder is pulled down. Usually when inferior and posterior instability, the patient may have generalised ligament laxity.
Instability can be divided up into the acute traumatic instability or chronic instability. The latter is more common in people with generalised ligament laxity (people who have a hyper-extensile ability eg they can hyper-extend the elbows, the fingers, the thumbs, the knees and are more likely to be able to dislocate their shoulders). Generalised ligament laxity generally tends to run in families and there may be a family history of previous shoulder dislocations or similar injuries such as cruciate disruptions. Any surgical repair for the shoulder is not going to correct the ligament laxity and thus makes them a higher risk of re-dislocation following surgery.
How is an episode of shoulder instability treated?
In the past, patients used to be treated with a sling for comfort and then rehabilitation. However there is evidence that following a first time dislocation, the shoulder has a much higher chance of re-dislocation. As such the re-dislocation rate in a patient under 35 years of age is associated with an 85% re-dislocation rate and in these patients, surgical repair is warranted. Those patients who decline it either because of work or sporting commitments and then go on to a second dislocation have close to a 100% re-dislocation rate. Surgery can reverse these odds and bring it down to approximately 10% re-dislocation rate. Unfortunately, no surgical procedure has 100% guarantee.
In a patient over 35 years, the chance of re-dislocation is a lot less and as such primary surgical procedures are not always indicated, and in the older patient the re-dislocation rate is not the main issue. What can occur in the older patient is a tear of the tendons around the shoulder. This needs to be always checked, particularly in an older patient who does not recover the strength following an initial dislocation.
Consequently, in the acute traumatic instability episodes, there are 3 main groups. There is a young person with a first-time dislocation, in which surgical intervention is warranted. There is a middle-age person, who may opt for a physiotherapy regime and non-operative approach. Finally, in the older patients there is a higher risk of tendon tear, and they may warrant surgery due to this risk.
What is the surgical procedure undertaken?
Generally, there are 2 types of surgical procedures that can be undertaken. There is the anatomical type repair where the soft tissue which has been pulled away from the socket is repaired, back to where it came from. This is usually undertaken with an arthroscopic procedure (keyhole surgery) using 2 or 3 holes to look in the shoulder joint, identify the area where the tissue has pulled away, roughen up the bone to stimulate healing to respond so that it will heal to the soft tissue and then insertion of 2 or 3 anchors (a small implant which have sutures attached to them). These are then used to tie the tissue back to the edge of the socket using arthroscopic techniques.
Following surgery, there is a 6 week period required in a sling to allow the tissue to heal and prevent extra stress being placed through it to avoid it re-tearing. There is a 6 month rehabilitation where the position of dislocation is avoided and strength is built up around the shoulder prior to returning to activities such as sport.
The other main type of reconstruction is a non-anatomic type reconstruction. This is one which is undertaken in someone who is high risk of re-dislocation or where there is significant bone loss from the socket; in other words, as the shoulder has dislocated the tissue has pulled away from the socket and has pulled away a bit of bone making the size of the socket even smaller than normal. In this scenario, a piece of bone from another aspect of the shoulder (the coracoid) is transferred to the front of the socket and secured with several screws. This piece of bone has a tendon attached to it which helps support the shoulder and prevents re-dislocation. It is a bigger procedure and does have a slightly higher risk of stiffness associated with it. It is also known as a Latarjet procedure.


What happens without corrective surgery?
If the shoulder continues to dislocate and if the edge of the socket scratches against the humeral head, it will lead to arthritis in the ball as it wears away the joint surface. Such patients are at high at risk of early arthritis.
Are there risks of shoulder reconstruction surgery?
Yes there are. The main risk is the risk of re-dislocation. You may be aware that some footballers who have shoulder stabilisation procedures then can continue to re-dislocate requiring more surgery. Unfortunately, in these patients they most likely have ligament laxity which makes them a higher risk. Certainly even in the best scenario shoulders can re-dislocate despite surgery. Other risks include risk of nerve damage, which can lead to weakness in part of the arm which may be permanent or usually is temporary. This is an extremely rare complication but can occur. There is also risk of the anaesthetic, as well as the time required off sport or manual duties at work. In general, shoulder instability is a very common event and if you are concerned you should seek advice from a specialist shoulder surgeon.
At Glenelg Orthopaedics, we have extensive experience in shoulder dislocations and instability. For more information, contact us.
